Exploring the history and evidence of the low-fat diet
Have you dropped the full-fat cream and opted for chicken breast to avoid weight gain and heart disease? In this first of a four part series I explain the fallacy of the low-fat and low saturated fat diet, outline some of the history of the public health policy to encourage the reduction of fat and saturated fat and describe why foods low in saturated fat aren’t always better for you, instead, exploring some of the benefits of lipids – fats, oils, and other fatty substances such as cholesterol and phospholipids.
.Saturated fat is good for you
We think of fat as a way our body stores energy for times of need (1, 2) and we have been led to believe in this era of caloric abundance and the epidemics of obesity and heart disease that we need to be avoiding or minimising fat and in particular saturated fat and the cholesterol that comes with saturated fat in foods of animal origin.
However, lipids have some important functions other than merely storing energy and as fat consumption in the U.S. has decreased both in absolute terms and as a percentage of caloric intake obesity has rocketed (3, 4).
The fat you do store in excess as adipose tissue is actually more complicated than we used to think and is now referred to as an endocrine organ as it produces hormones and inflammatory molecules (‘cytokines’) that seem to contribute to the diseases associated with obesity, such as cardiovascular disease, type 2 diabetes and chronic kidney disease (5) as well as nonalcoholic fatty liver disease (6).
Foods low in fat and saturated fat aren’t always better for you
However the storage of more fat does not necessarily come from fat consumption and many of the conditions previously linked to a high fat diet may be more reflective of total caloric intake (7). In fact the low fat diet and foods low in saturated fat encourage eating more carbohydrates which has increased the prevalence of obesity (8). Carbohydrates cause your body to release more insulin which stores the calories from carbohydrate as fat (9, 10) which is perhaps part of the reason why a low carbohydrate diet may be generally more effective for sustained weight loss than a low-fat diet (11) although higher protein intake is perhaps also a major factor (12).
High fat diets and increased fat burning and satiety
Moreover fat-burning is increased on a high-fat diet (13) and the fat burning benefits of exercise are reduced on a low-fat diet (14). Energy availability after meals on a low-fat diet is decreased relative to a low glycemic diet and a very low carbohydrate diet, and together with reduced metabolic rate compared to the very low carbohydrate diet could contribute to rebound weight gain (15).
Carbohydrate is also less satiating than fat so that reducing fat is likely to cause an increase in the total number of calories consumed and hence weight gain (16).
A paleo type diet, based on meat, fish, fruit, vegetables, root vegetables, eggs and nuts, has been found to be more satiating than a low-fat diet (17) and can be very effective for weight loss (18, 19, 20).
Low-fat diet, low saturated fat diet and heart disease
I have already explained how the low-fat diet may actually cause weight gain which is associated with an increased risk of heart disease.
The evidence for saturated fats causing heart disease is in fact very weak (21, 22) and refined carbohydrates pose a much more significant risk to heart health than saturated fat (23).
Switching to a high-carbohydrate low-fat diet whilst consuming the same amount of total calories increases blood triglycerides (fats) (24) which are a risk factor for heart disease (25), and as I have already stated, replacing fats with carbohydrates is likely to result in increased caloric intake so the effect on triglycerides in practice is likely to be even greater. The paleo diet tends to improve markers of heart disease risk by increasing HDL, whilst reducing LDL and triglycerides, whereas the grain-based diet recommended by the American Heart Association which replaces saturated fat with carbohydrates and reduces total fat intake can worsen these markers of heart disease risk (26).
Hunter-gatherer diets tend to be high in animal fat and lower in carbohydrate and hunter-gatherers have been found to be ‘generally free of the signs and symptoms of cardiovascular disease’ (27).
Other aspects of the hunter-gatherer diet and lifestyle are also likely to contribute to improved heart health, such as the higher omega-3:omega-6 fatty acid ratio, higher protein, fibre and phytochemical intake, more exercise, less chronic stress and no smoking, but the absence of heart disease in hunter-gatherers should at least tell us that animal fats in and of themselves are not likely to harm your heart and that therefore the consumption of foods low in saturated fat isn’t directly related to heart health.
Postmenopausal women placed on a low-fat diet for a mean of 8.1 years as part of the Women’s Health Initiative did not significantly reduce their risk of heart disease and stroke despite an increased intake of fruit and vegetables although grains were also increased (28) and may have had a negative impact.
The PURE study published in 2017 tracked 135,335 individuals in 18 countries over a median of 7.4 years and linked higher carbohydrate intake to increased mortality and higher intake of total fat, or any type of fat (saturated, monounsaturated or polyunsaturated) was associated with reduced mortality. No association was found between total fat and heart disease or any type of fat, be it saturated, monounsaturated or polyunsaturated, and heart disease, although higher saturated fat intake was associated with a reduced risk of stroke (29).
The ketogenic diet, lipids and heart disease
Indeed we might expect higher carbohydrate intake to be associated with increased mortality since low carbohydrate diets have been used to improve the most important cardiovascular risk factors. Concerns about higher levels of LDL cholesterol on ketogenic diets are unfounded, since most individuals on such a diet will not experience a clinically significant rise in LDL cholesterol, and although there may be a small increase in LDL cholesterol on average, the number of LDL particles and small, dense LDL particles are decreased (30), as is the triglyceride to HDL ratio (31) and these are far more reliable markers of heart disease risk, as explained here.
Indeed there are some individuals whose LDL cholesterol on a ketogenic diet rises to levels that are considered dangerous, and it has been found that this rise is associated with leanness and a low triglyceride to HDL ratio. In fact the more lean an individual and the lower the triglyceride to HDL ratio the higher the rise in LDL cholesterol when carbohydrate intake is restricted. The “lean mass hyper-responders”, as these individuals have been named, saw a decrease in LDL cholesterol back to normal levels when dietary carbohydrate was then increased (32).
So what is going on here? Are these hyper-responders with their baseline low-risk cardiovascular disease markers suddenly at risk of heart disease on a low carbohydrate diet because increased saturated fat intake is increasing their LDL cholesterol, although other risk factors remain low? Our information on this is limited, but in one case study a lean hyper-responder was on a more Mediterranean style of ketogenic diet, with a high intake of oily fish and olive oil resulting in 82% of fat intake being monounsaturated or polyunsaturated and just 18% saturated. When this individual increased saturated fat to 45% of fat intake there was little impact on his LDL cholesterol levels. Despite sky-high LDL cholesterol levels for 2.5 years a CT angiogram revealed no formation of arterial plaque, indicating no heart disease (33).
However, could this one individual have been an outlier, with an atypical response, perhaps due to his genetic make-up or some other unknown factors? Perhaps that could yet turn out to be the case, but a study currently underway on 64 hyper-responders on a ketogenic diet with LDL cholesterol levels in the top 0.1% of the (US) population for 4 years indicates 2/3 of the participants have zero calcification or plaque in their arteries, and the remainder have a low plaque score (34).
So although I have indicated that perhaps heart disease risk is not increased and saturated fat is not a risk according to preliminary data, I have not yet explained what might be causing the high LDL cholesterol and yet low triglyceride to HDL cholesterol ratio in lean mass hyper-responders on a ketogenic diet. A hypothesis has been proposed which requires a little background explanation as follows, but it may also be helpful to read my description in another post of what lipoprotein particles are and whether cholesterol causes heart disease.
On a ketogenic diet one is more dependent on fat stores in the adipocytes (fat cells) than glycogen (the storage form of glucose) in the liver and muscles. After a meal the adipocytes become larger and then they give up their fat and become smaller as the energy supply from the meal gets used up by the tissues. All of this requires lipoprotein particles to carry the fat around in the bloodstream, since fat and water do not mix. The liver packages these lipoprotein particles with fat and releases them into the bloodstream. As the fat (in triglyceride form) gets rapidly taken up by the tissues the lipoprotein particles get smaller and denser and now become LDL lipoproteins and HDL lipoproteins that carry cholesterol, so called LDL cholesterol and HDL cholesterol. When we speak of blood triglycerides it may sound like the fat is just dissolved in the blood, but in fact it is also transported in such specialised fat-transporting particles.
The adipocytes are efficient ‘professionals’ at taking up and releasing fat, but there is a maximum size they can reach and what happens when they are full? At that point any excess calories as triglycerides (fat) get stored in other tissues, such as your liver (causing fatty liver), heart, kidneys, pancreas and muscle tissue (35). This ‘ectopic’ (out of place) fat tissue is not as efficient at taking up and releasing fats as the ‘professional’ adipocytes, and so in overweight individuals with poor metabolic health circulating triglycerides will be high, in contrast with the lean mass hyper-responders in whom the adipocytes rapidly and efficiently take up the triglycerides from the bloodstream. You could think of the high (blood) triglycerides in the metabolically unhealthy individual as the result of calorie intake exceeding calorie storage sites, so that the body use the blood (the transport system) as a last resort for storage. One of the authors of the hypothesis uses the analogy of ships loaded full with cargo but with nowhere to drop the cargo off due to lack of demand (36).
For the sake of brevity I have tried to outline a complex subject in a very simple way here, but for a more comprehensive explanation you could read the original hypothesis or watch the explanatory videos linked in the references (37, 36, 38, 39).
More evidence fat and saturated fat do not cause heart disease
A 2014 review of over 70 studies found no difference in mortality from heart disease in those eating a higher saturated fat diet when compared to those eating a lower saturated fat diet (40). A 2015 meta-analysis found that restricting dietary fat did reduce cholesterol but not mortality from hearty disease or mortality overall from all causes (41).
So for most people saturated fat is unlikely to cause harm and may even reduce the risk of stroke, although the minority of us with familial hypercholesterolaemia or the APOE4 genetic variant might in fact benefit from not eating too much saturated fat as explained in my posts on cholesterol.
Lower levels of cholesterol are in fact associated with increased mortality (42) and I have previously outlined 10 reasons you need cholesterol and in this series I will focus more on fats and oils.
The history of the low-fat and low saturated fat diet
So where did the message come from that fat and saturated fat in particular cause heart disease?
Before the birth of the U.S. vegetable oil industry in the 1940s imported coconut oil, which is primarily saturated fat, was the main source of plant-based fat in the USA (43) and economic interests may have driven the campaign against saturated fat more than concern over public health (44, 45).
One of the most (in)famous studies to claim to find a correlation between fat intake and heart disease rates included this graph of 6 countries plotted by Ancel Keys in 1953 (the annotations in red are mine).
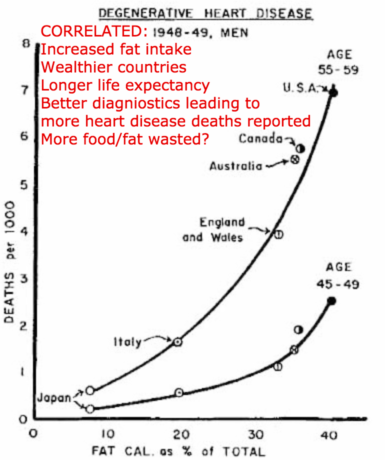
A correlation between wealthier countries and higher fat intake
However the correlation really reflects a correlation between wealthier countries and higher fat intake, better diagnostic reporting of heart disease as such in these wealthier countries thus pushing up the heart disease numbers despite an overall longer life expectancy in the wealthier high fat countries, and the interpretation is further skewed by calculating diet data from national export, import and production statistics when you would think far more food would go to waste in the wealthier nations (46).
Ancel Keys for some reason also only used data from 6 countries. If he had used the data from all 22 countries that was available at the time the graph would have looked like this.
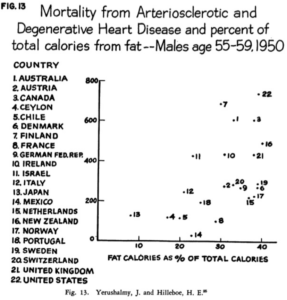
You can see the correlation is weaker when all 22 countries are included.
In 1957 a committee of the American Heart Association rejected the theory that replacing saturated fat with PUFAS from the new U.S. produced vegetable oils would reduce heart disease risk. However, only four years later, after Ancel Keys and three other new members became two thirds of this committee, the recommendation was then made for men at risk of heart disease to replace some of their saturated fat intake by polyunsaturated fat, despite no new evidence coming to light since the previous committee had rejected this proposal four years earlier.
The sugar industry is now known to have further manipulated the science in the 1960s (47) and the resulting low-fat diet has led to an increase in refined carbohydrate intake which has been one of the main drivers behind the explosive rise in obesity and type 2 diabetes over the 40 years of reduced fat intake that followed (48).
The low-fat fallacy: the series continues…
So I have briefly described how the low-fat and low saturated fat diets came to be promoted despite a lack of evidence for their efficacy in achieving their stated purposes either in reducing heart disease risk or for weight loss. I have also outlined some of the mechanisms that could explain the huge increase in obesity in the USA despite of or in fact because of the reduction in fat consumption both in absolute terms and as a percentage of total caloric intake. In the next three posts I will outline some more benefits of lipids and fatty foods for the health of your body and brain and in the final post I will also mention how fat can benefit beauty and will give some advice on how much fat to include in your diet.
What has your experience been with fat and saturated fat in your diet? Did your grandparents or even your parents follow the same diet they did before before the low-fat message was so heavily promoted, and how do you feel their health may have been affected?
Read Part 2, learn more about my work in London and Totnes, or find out about online consultations.
SIGN UP TO THE NEWSLETTER TO BE NOTIFIED WHEN EACH NEW POST IS RELEASED.






Another great video Tom.
You have mentioned the APOE 4 allele in this video and previous video’s regarding it’s genetic influence on how fat is metabolised. The FADS2 gene is another gene that has evidence in how it effects how ALA converts to EPA, so there are gene’s that can have an influence on certain fats. Is there any particular gene’s that effect the body/metabolism in similar way with carbohydrates and Protein?
Thank you Andrew.
Of course every gene codes for a protein to be built from amino acid so we have genes for detoxification enzymes such as CYP1A2 which metabolises caffeine and antioxidant enzymes such as catalase, which are proteins, for example. There are quite a few genetic variants that increase the tendency to blood sugar imbalances, such as GLUT4 which regulates glucose uptake in muscle.