Nutrition and nutritional therapy for gut health
Learning about nutrition for gut health as described in this article can help you with your IBS, IBD, SIBO, candida overgrowth and other gut conditions. However, this generalised advice applied at the wrong time can sometimes also be harmful as it depends on various factors, such as what is causing your IBS, whether you are in an active flare of IBD or not or whether SIBO is causing you to be sensitive to certain foods that could otherwise support the heath of your gut and of your microbiome.
For a more individualised approach you can also read about how I utilise the tools of functional medicine, naturopathy and nutritional therapy for gut conditions in my Wisdom Nutrition gut health clinic in London, Devon (Totnes) and online.
Why focus on nutrition for gut health?
Nutritional therapy, naturopathy and functional medicine work with nutrition for gut health, but also take into account lifestyle factors such as stress. In this article you will learn why nutrition is so important for gut health, and how your nutrition, your gut lining and your gut microbiome all interact to maintain gut health and overall physical and mental health beyond the gut.
Based on this understanding nutritional therapy, functional medicine and naturopathy can provide effective support both for the many conditions that can originate in the gut without necessarily causing digestive symptoms and also for chronic gut conditions with clear digestive symptoms.
Nutrition for gut health for nutrition – a 2-way street
Gut health and nutrition have a bidirectional relationship in that nutrition not only affects gut health but gut health affects the absorption and metabolism of nutrients, as will be explained below.
Why improve gut health?
For those who have not experienced them chronic gut conditions such as IBS may appear to be minor ailments, but symptoms such as bloating, constipation, diarrhoea, flatulence, abdominal pain or discomfort, acid reflux and heartburn can seriously impact your quality of life.
More severe conditions such as Inflammatory Bowel Disease (IBD) severely impact quality of life, drive inflammation and nutrient malabsorption, and thus increase the risk of osteoporosis and arthritis.
Aside from the obvious digestive discomfort, gut conditions are associated with fatigue (1), insomnia, anxiety and depression (2), osteoporosis, skin conditions & joint pains (3), headache (4), cognitive dysfunction (5), vitamin and mineral deficiency due to malabsorption (6) and even conditions such as Autism Spectrum Disorder (7) and ADHD (8).
Elsewhere I have described how overuse of painkillers can worsen headaches in the long-term, and how a key step in the mechanism of this effect is that painkillers cause a ‘leaky’ gut.
Gut imbalances can adversely effect every system of the body: immune function (9), thyroid function (10), adrenal function (11), oestrogen levels (12), liver (13) and kidney (14) function, cardiovascular (15) and bone health (16). They even affect energy production at the subcellular level in the mitochondria, the powerhouses of your cells.

The immune system in your gut
Usually we think of immune cells as located in the blood and lymph, but 70-80% of your immune cells are in your gut wall.
Your gut wall is an important barrier designed to allow molecules of food in and to keep pathogens out, with immune cells acting as sentinels to monitor the environment in your gut. These immune cells in your gut wall communicate with your systemic immune system, which refers to your immune system throughout your whole body rather than in a localised area.
The gut microbiome also affects your systemic immune system and a key factor that determines your gut microbiome is your diet (17).
Gut microbiome and weight loss
Your gut microbiome has also been linked with fat storage. The kind of gut microbiome that increases fat storage has been found to predominate in colder climes, where it offers a survival advantage (18).
Growing evidence indicates that an imbalanced gut microbiome can result in the release of bacterial toxins from the gut entering the bloodstream which can drive inflammation elsewhere in the body, potentially resulting in obesity, blood sugar dysregulation and the arterial plaque that is a hallmark of cardiovascular disease (19, 20).
The gut-brain axis
In recent years there has been a growing body of research on the bidirectional channel of communication between the gut and the brain known as the ‘gut-brain axis’.
Your gut flora can communicate with your brain and are important for healthy brain function. Thus if we can improve the health of your microbiome we can potentially also reduce anxiety, depression and stress (21).
The gut-brain axis is bi-directional, since there are also many ways in which stress affects your gut.
We now know that inflammation in the gut can cause inflammation in the brain and vice versa.
The gut-brain-skin axis
The link between depression, anxiety and skin conditions such as acne has long been observed.
As far back as 1930 it was proposed that depression and anxiety could caused an altered gut microbiome and hence ‘leaky gut’ and inflammation.
More recently the pieces of evidence are falling onto place to support this hypothesis not just for acne but also for psoriasis, rosacea and eczema (22, 23, 24, 25).
Epigenetics – How your gut microbiome will affect your grandchildren
Epigenetics refers to the expression of genes, meaning which genes are turned on or active, and which are turned off. Epigenetics can have a profound effect on your health. The epigenetic markers that activate or deactivate particular genes can be passed down through the generations, and are another way besides the genes themselves in which parents can pass down tendencies toward health or disease to their children and even to their grandchildren. Unlike genetics, however, you can influence your epigenetic profile for your own benefit and for the benefit of future generations. This is another area in which gut health plays a role, as we now know that the gut microbiome has an impact on your epigenetic profile (26).
Why work with nutrition for gut health?
There is plenty of evidence that nutrition affects health in many ways.
The fact that food enters the body through the gut should in itself be enough to highlight the central role of the gut in general health, though as you read on you will learn more about some of the ways in which the health of your gut and of your microbiome are crucial to overall physical and mental health.
Whether working to improve your gut health alone or with the guidance of a nutritionist, dietary changes are known to profoundly impact your gut n many ways. This approach avoids the risk of potential harm to your microbiome or to your gut with approaches that simply rely on stronger interventions such as antimicrobials or laxatives, be they herbal or pharmaceutical, without nourishing your gut microbiome.
How nutrition feeds your gut microbiome
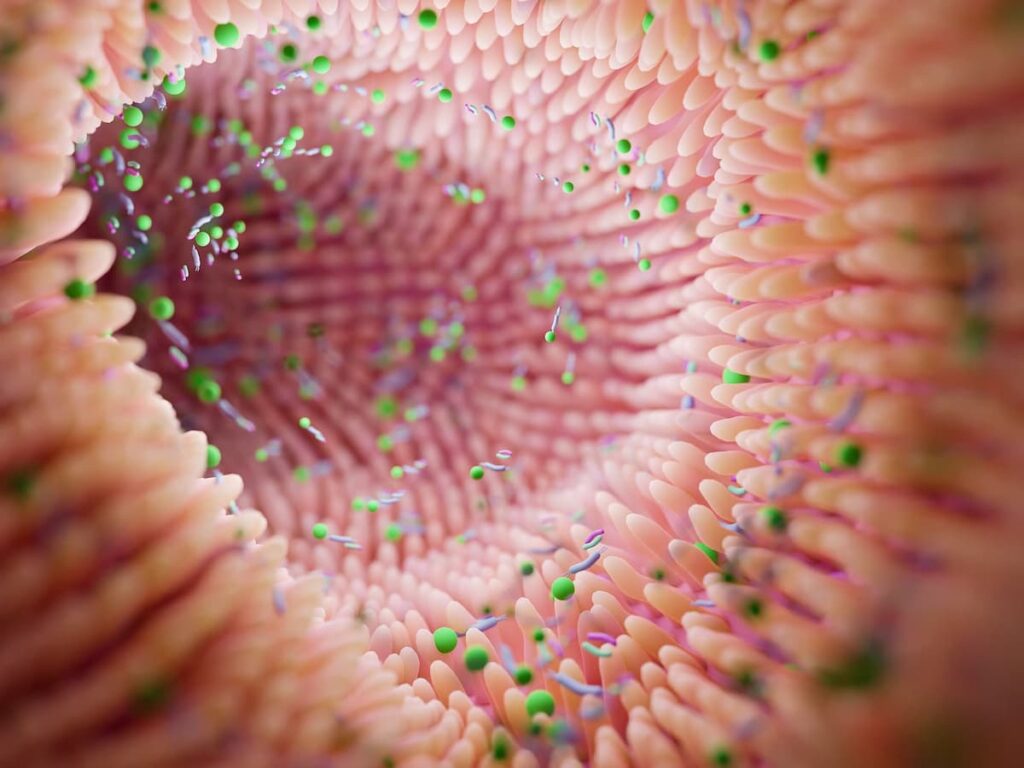
Of the food that you eat what ‘you’ don’t digest is digested by your gut microbiome. I put ‘you ‘ in quotation marks because it is arguable as to whether your gut flora are really separate from ‘you’, since they support your health in so many ways and since they outnumber the living cells in your body that are not bacteria (27). Having said that, it is also often said that your gut lining forms a barrier between you and the outside world, the importance of which is discussed below.
Since fibre is not digested by ‘you’, you would be right to think that fibre is a key nutrient for your microbiome, but nutrition for your microbiome also includes the macronutrients carbohydrate, protein and fat, which are not completely digested by the digestive enzymes produced by your human body, such as those made in the pancreas.
Even dietary micronutrients – vitamins and minerals – have an impact on your gut microbiome. Since your gut flora produce some key micronutrients and affect micronutrient balance and absorption in other ways, nutrition for your microbiome also supports nutrition for yourself.
Gut dysbiosis and gut microbiome diversity
There is a complex web of interactions between different species in your gut microbiome that we are just beginning to understand. One species, for example, may digest certain kinds of molecules from the food we don’t digest and produce from these metabolites that benefit other species. Species can also engage in chemical warfare to keep each other in check, but we don’t want one species to win the war and to dominate your microbiome.
Gut dysbiosis is when your gut microbiome deviates from a healthy composition and the diversity of species is decreased. Perhaps just a few species dominate and crowd out other species.
To get a sense of why diversity is important we could think about forests.
On the one hand we have a pine forest, which is very uniform and in which few other species can survive. On the other hand imagine countless species of flora and fauna each occupying a specialist niche and interacting with other species to maintain the overall balance of a tropical rainforest.
A healthy gut microbiome, then, is like a vibrant rainforest.
A healthy gut microbiome helps to prevent disease
A healthy gut microbiome will also help prevent pathogenic (disease forming) microbes from colonising your gut.
Healthy species produce antimicrobial substances and compete with pathogens for food and physical space to occupy on the gut wall and also improve your immune response to pathogens (28).
This is why, for example, antibiotics can reduce colonies of beneficial species and lead to the overgrowth of species of bacteria (clostridia difficile) that can lead to Inflammatory Bowel Disease, such as Crohn’s disease or ulcerative colitis (29).
Gut dysbiosis causes ‘leaky gut’ which causes inflammation
Your gut lining forms a barrier between yourself and the outside world, and needs to allow digested food particles in whilst keeping undigested food particles, toxins and pathogens out of your blood stream.
You could think of your gut barrier as a sieve with a certain grade of mesh to keep out larger particles. It is a healthy microbiome that helps to maintain a healthy gut barrier, whereas gut dysbiosis can cause larger holes can form in the sieve and you are left unprotected from the undigested food particles, pathogens and toxins that can now enter your bloodstream, and this is often referred to as ‘leaky gut’.
The result of the leakage into the bloodstream is inflammation in other parts of the body, which is one reason why gut dysbiosis can cause symptoms elsewhere in the body as discussed earlier, and this can happen even if the absence of any symptoms in the gut itself.
Toxins may be environmental, entering your gut in your food supply, but toxins from bacteria in your gut that manage to enter your bloodstream are now known to be a key driver of inflammation and chronic disease.
Toxins from a fermenting gut, such as alcohol and acetaldehyde from an overgrowth of candida albicans and other fungal species, can have also a strong impact on your body and brain as any drinker will know, and are a major cause of brain fog, anxiety, depression, insomnia or sleep disturbances, aches and pains, skin complaints such as rashes and many other symptoms that could potentially manifest in the gut or outside of the digestive system.
Gut microbiome, leaky gut, food sensitivity, allergy and autoimmunity
Since your gut lining forms a barrier between yourself and the outside world, it is rich in cells that are seen as part of the immune system.
Some of these cells sample what is in your gut and send appropriate messages to immune cells in your blood stream and elsewhere in your body. Your gut bacteria also play a role in this signalling, which therefore depends on a healthy gut microbiome.
These signals let your immune system as a whole know whether it needs to respond to pathogens, toxins or undigested food particles by mounting an inflammatory response, which also skews your immune system in a certain direction.
Equally important are signals to calm down the immune response. Gut dysbiosis can cause this aspect of signalling to fail. The resulting over-reactive inflammatory immune response can cause food sensitivity, allergy and autoimmunity.
Nutrition for gut health – directly and indirectly feeding your gut lining
Another way in which good nutrition supports gut health is by feeding the cells lining your gut. These cells are replaced every 3-4 days and you feeding them adequately can support healing a leaky gut.
Glutamine – nutrition for the small intestine
The amino acid glutamine is the primary fuel for the cells lining your small intestine and can only be provided from the protein you eat, or from supplements, though glutamine supplements should be used under professional supervision as they do have the potential to cause harm.
Butyrate – nutrition for the large intestine
The cells lining your large intestine are fed indirectly. Certain species of bacteria ferment dietary fibre to produce short chain fatty acids.
One of these short chain fatty acids is butyrate, which is the main fuel source for the cells lining your large intestine.
Butyrate is so named because it is found in butter. If you have noticed that ghee (from dairy not vegetable ghee) has an odour that might remind you of vomit, that is because ghee and vomit are both rich in butyrate. (It’s always good to relate these concepts to personal experience).
Butyrate health benefits for the gut
In the gut itself butyrate improves gut motility to reduce constipation, helps to heal an inflamed gut wall and keeps the large intestine slightly acidic which allows beneficial gut bacteria such as lactobacilli and bifidobacteria species to flourish. These bacteria can help to keep fungal overgrowth at bay, but butyrate is in itself directly antifungal.
Further health benefits of butyrate beyond the gut
Butyrate has many other health benefits beyond the gut. It helps to reduce inflammation and provides an alternative fuel source not just for your gut but for the rest of your body and increases satiety when you are going without food. Butyrate supports your mood by boosting neurotransmitter production, supports healthy blood sugar regulation and weight loss.
Why butyrate production may be low
Stool analysis often reveals low levels of butyrate. This can be from a lack of dietary fibre or from gut dysbiosis, since only certain species produce butyrate and some other species, such as hydrogen sulphide producing bacteria, can reduce butyrate production.
Acetate – nutrition for the gut immune system
Acetate is another short-chain fatty acid that primes the immune system against gut pathogens, thus reducing the risk of gut dysbiosis.
A high fibre diet in mice has been shown to increase acetate production which primes both immune cells and cells of your gut wall against the dangerous bacterium clostridia difficile, so called because it is difficult both in the symptoms and potential complications it can cause and in its resistance to treatment (30). (Actually I am using the old name for a bacteria that has been renamed as clostridoides difficile, but if you have heard of it you probably still know it by the old name, as the new name has not yet caught on except in the research literature).
Acetate also stimulates the repair of your gut wall that has been damaged by toxins produced by clostridium difficile (31).
Healthy nutrition choices for your gut
Why gut-healthy foods could be making your gut condition worse
You may well be reading this because you are suffering from symptoms of a chronic gut condition or because you have another condition that may be related to gut health. In that case you may have already realised that certain foods exacerbate your symptoms and you may have reduced or eliminated these from your diet.
You may be surprised that some of these foods are commonly recommended for gut health. These are the prebiotic foods that contain fibre that is a fuel for your microbiome.
If you react to these it may not be due to a food sensitivity, which is when your immune system responds to the food as described above. It may instead be a sign of gut dysbiosis and the healthy foods that normally act as fuel for your beneficial gut flora are instead feeding an overabundance of more inflammatory species, which could include not only bacteria but parasites and fungi like candida albicans.
Nutrition for a healthy gut
Diversity of plant foods for microbiome diversity
If your gut is reasonably healthy eating a wide variety of plant foods with various fibre types will provide fuel for different species of gut bacteria (and for butyrate production) and thus promote the sought after diversity of species in your gut microbiome. To eat a sufficient quantity of these foods a guideline is to fill 3/4 of your plate with non-starchy vegetables at every meal, and to vary your source of starchy foods which should be from unrefined plant sources such as tubers, whole grains and pulses (legumes such as beans, chickpeas and lentils). You could increase the types of plant food plant foods you eat by including various nuts and seeds in your daily diet.
You can further increase the diversity of your plant foods (and thus the diversity of your gut microbiome) by ‘eating the rainbow‘, which means eating from each colour group. You can then move on to eating 30 different plant foods a week, which is not as difficult as it might seem.
Prebiotic foods for gut health
You could also make sure to include more prebiotic foods when choosing both starchy and non-starchy vegetables. Prebiotics are food components that feed your gut microbiome and prebiotic rich foods include:
However every plant food and even unicellular algae like spirulina and chlorella will have a prebiotic effect, and in my view it is better to widen your focus onto a diversity of plant foods than to fixate on large quantities of more strongly prebiotic foods.
Polyphenols as prebiotics
One of the reasons plant foods benefit health is due to the antioxidant compounds known as polyphenols, which often give foods their colour. The main reason for ‘eating the rainbow’ as described above is actually to provide a wide range of polyphenols and other beneficial pigments.
Besides all their many other health benefits, polyphenols tend to improve gut health by acting as a prebiotic to feed the bacteria that support gut health and by reducing numbers of bacteria that are harmful to your health.
Fermented foods for gut health
Fermented foods can act as probiotics, meaning they can be a source of live bacteria that can support gut heath and in particular the health of your gut microbiome.
Here it is important to focus on live fermented foods which have not been pasteurised or cooked such as sauerkraut, kimchi, yoghurt, kefir, pickles and miso. You can sometimes tell a real live sauerkraut as it can bubble away, as I have seen many times with an organic brand currently found in most UK health food shops.
Tempeh cannot be eaten raw so it won’t benefit you as a probiotic food but can act as a prebiotic food.
I would hesitate to recommend kombucha, until there is further evidence of health benefit.
Nutrition for gut dysbiosis
If you have gut dysbiosis the one-size fits all approach discussed so far could make your symptoms worse, whether or not your symptoms manifest in your gut, in your brain as poor cognitive function, depression or anxiety, or elsewhere in your body.
The prebiotic foods in particular could exacerbate your symptoms by feeding the microbes in your gut that are already dominant. Eating larger portions of plant foods could worsen your gut because you will be increasing prebiotic foods.
This is where professional support with a suitably qualified and experienced functional medicine practitioner, naturopath or nutritional therapist can determine, with the help of lab testing, which foods and lifestyle changes could help to heal your gut and what are the underlying causes of your poor gut health. There are numerous types of diet suitable for individuals with various sensitivities caused by different factors, some of which are not obviously related to gut health.
There is some limited general advice that can help some people with gut dysbiosis, however. Some of this advice will only apply if you have dysbiosis that is exacerbated by foods high in prebioitics.
Firstly stopping gluten grains such as wheat, barley, rye and triticale and dairy produce (except for butter and ghee) can be helpful. Note that spelt and kamut are types of wheat and should also be included.
Whether or not this improves your gut due to the reduction of gluten and the milk protein casein in your individual case is another question. Although both gluten and casein are gut irritants and will cause leaky gut and hence gut dysbiosis (32), gluten grains and dairy produce are rich in prebiotics. Because the risk versus benefit analysis is not easy to make in general I did not include these foods in my list of prebiotics.
In the case of dairy produce the prebiotic is lactose, which many people are sensitive to, as they can be to gluten and casein.
Reducing your intake of high prebiotic foods from the list above may actually be helpful in the short term if you have gut dysbiosis, although the goal would be to replenish your gut microbiome with prebiotic foods when you can eventually tolerate them, and because of the risks to your microbiome involved professional support is recommended.
So how can you support your beneficial gut flora whilst not feeding the dominant dysbiotic gut flora?
Firstly you need to understand that the favourite food source of most of the dysbiotic bacteria, fungi and parasites is carbohydrate, and especially refined carbohydrates and sugar, so experiment with reducing your portion sizes of starchy foods, focus on whole foods and consider eliminating sugar in all its forms altogether. You will probably need to avoid sugar even in the form of fruit.
In case you are concerned, there is nothing essential to your nutrition in fruit that you cannot find in other plant foods.
Many gut conditions benefit from reducing or avoiding caffeine, alcohol, ultra-processed foods and food additives. Some people’s guts are also sensitive to the antibiotics in conventionally reared meat and in farmed fish.
After reducing or eliminating these foods you can then do your best with the foods you do tolerate. You may want to experiment with avoiding or reducing some of the more prebiotic foods for a few days or a week just to see if this improves your symptoms.
Since polyphenols tend to improve gut flora by acting as a prebiotic for desirable bacteria and as an antimicrobial for less desirable microbes, you could focus on the deeply coloured plant foods higher in polyphenols but avoiding or limiting the higher prebiotic foods.
Fermented foods may be helpful, but for various reasons beyond the scope of this article some people react to them.
Nutrition and lifestyle changes for gut health
You should now understand the importance of nutrition for gut health. However, besides being a nutritionist I also work with functional medicine, naturopathy and nutritional therapy. These modalities also look for changes we can make to improve health beyond nutrition. and there is plenty of evidence for the power of lifestyle changes to also impact gut health.
Nutritional therapy for gut health in London, Devon and online
Functional medicine, naturopathy and nutritional therapy look for the root causes of gut conditions.
Health questionnaires, diet diaries and further questions during consultations regarding your symptoms, medical history, family medical history, previous test results, lifestyle, sleep patterns, stress levels, toxic exposures and more all help to guide me towards the most likely root cause or root causes that need to be addressed in order to heal at a deeper level rather than just offering symptomatic relief.
Nutritional therapy for gut health – functional testing
Functional medicine and nutritional therapy for gut health also incorporate lab testing to provide evidence as to the root causes of gut conditions. This information guides us towards the most effective nutritional interventions to improve your gut health. Functional lab testing for gut conditions could include:
- Stool testing
- Breath testing, such the lactulose breath test for SIBO
- Urine testing – the Organic Acids Test and the 24 hour urine oxalate test
- Blood testing – for candida antibodies of for antibodies involved in food sensitivities
- Micronutrient testing – since gut conditions can both cause micronutrient malabsorption and be affected by suboptimal micronutrient levels
The causes of gut conditions may not always lie in the gut itself, so a wide variety of further testing may be appropriate, including saliva, blood, urine and even hair testing.
Functional and genetic testing may be helpful for determining the most effective support for chronic gut conditions such as:
- Irritable Bowel Syndrome (IBS)
- Small Intestinal Bacterial Overgrowth (SIBO)
- Intestinal Methanogen Overgrowth (IMO)
- Fungal infection such as candida overgrowth
- Parasitic infections
- Bacterial infections, including clostridoides difficile, FKA clostridia difficile
- Crohn’s Disease
- Ulcerative colitis
- Acid reflux (GERD/GORD)
- Intestinal permeability (‘Leaky Gut’)
- Food intolerance or food sensitivity
- Chronic constipation
- Chronic diarrhoea
Book a free no-obligation 20-minute telephone appointment using the form to the right to find out more about how I can support you to improve your gut health, or click on the Services & Prices menu above to find your way to more information about how I apply the principles of functional medicine, naturopathy and nutritional therapy in my London, Devon and online clinics.





